
At rheumatoid arthritis, which is a systemic rheumatological disorder affecting multiple joints. The clinical presentation of rheumatoid arthritis is arthritis, which is symmetrical. We have pain, swelling, as well as nodules around the area. Hand involvement is early in the disease and affects the metacarpophalangeal and proximal interfalangeal joints.
In rheumatoid arthritis, there’s also extraarticular involvement, which we will look at later on. But first, let us look at the hand involvement in rheumatoid arthritis and see how it differs to osteoarthritis. So here is rheumatoid arthritis and osteoarthritis. So in osteoarthritis, the joints affected are the distal interflangeal joints, as well as approximal interflangeal joints, whereas in rheumatoid arthritis, it is approximal interflangeal joints and the metacarpophalangeal joints as well.
You can have other joint involvements, such as the wrist. So these joints are affected early in the disease. In rheumatoid arthritis, but as the disease progresses, you can have other features occurring in the hands. These are swan neck, butonier, or z deformity of the thumb. So in Swannick, what you have is you have the distal interflangeal joints flexed, but the proximal interflangeal joints hyperextended.
In boutonniere, it’s the opposite. You have the distal interflangeal joints hyperextended and the proximal interflangial joints flexed. The z deformity of the thumb is essentially the thumb looking like a z. It’s sort of bent, hyperextended in the hands. The hands can also deviate medially.
This is referred to as ulna deviation. So they were the features of the hands in rheumatoid arthritis. Let us actually look at what happens inside the joints. So let us zoom into a finger here, and just to recap the anatomy, here we have the bone, the joint capsule, the synovial membrane, also known as a synovium.
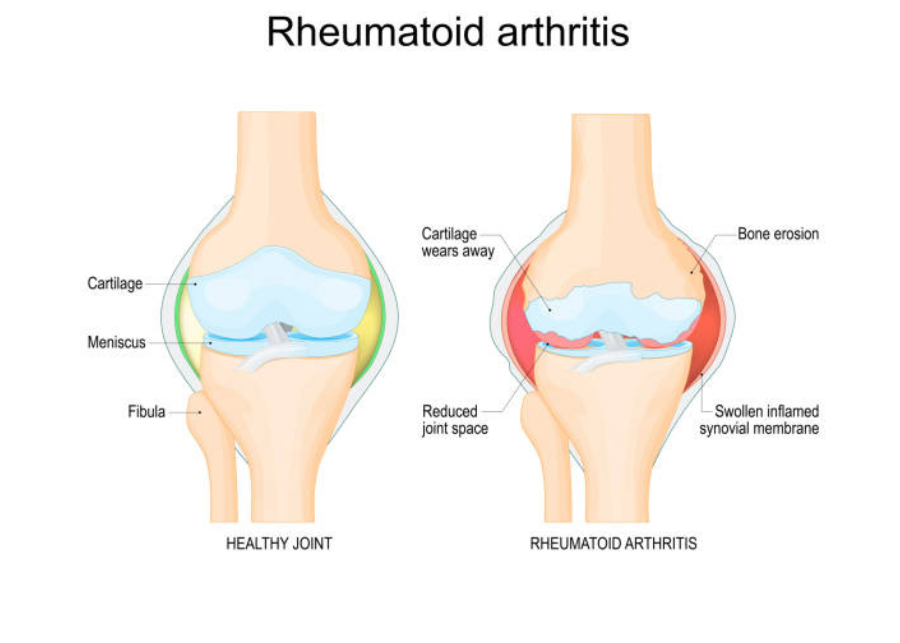
The synovial membrane, also known as a synovium, which produces the synovial fluid, which helps in lubrication as well as supplying nutrients to the area. Then we have the cartilage here in blue. In rheumatoid arthritis, you essentially have inflammation of the synovium of the synovial membrane.
You have sinovitis, and this causes pain and swelling, which occurs in rheumatoid arthritis. This also leads to bone and cartilage erosion, breakdown. Another feature we can see in the joints of rheumatoid arthritic patients is angiogenesis. So that was the macroscopic view of the joint. Just an overview. Let’s look at it in a lot more detail at a cellular level. Let us zoom into this area and see what cells are involved.
So just to show where we are, here we have the bone, the synovium. Here is the fluid. Here in yellow and blue is the cartilage. And again, I’m drawing the synovium really big because it is inflamed. Right. The synovial membrane. Now, the synovial membrane is made up of these cells, known as fibroblast like synoviocytes. And these guys are very important in the pathogenesis of rheumatoid arthritis.
So, again, rheumatoid arthritis is where we have inflammation of the synovial membrane of the synovium. Now, the exact trigger of the inflammation of the disease is really not quite known. However, we are now looking at what cells we can find here and what cells are involved. So we have macrophages here, and they’re normally around here as well, but they essentially begin secreting cytokines, such as tnf alpha, interleukin one, and interleukin six, which, of course, leads to inflammation. These cytokines also stimulate the fibroblast like synoviocytes.
When the fibroblast like synoviocytes are stimulated, they essentially become activated, and then they begin to proliferate. At the same time, they also begin assisting in rank l expression, stimulating the rank l expression, which, together with the cytokines here, will stimulate osteoclast activity, which will lead to bone erosion. What we find in rheumatoid arthritis, when the fibroblast like synoviocytes are stimulated and proliferate, they also begin secreting proteases.
These proteases essentially cause the cartilage to break down, so we get cartilage degradation, and the cartilage also secrete proteases, and it’s sort of like a feedback loop. Another interesting feature of the fibroblast like synoviocytes is that when it’s stimulated, when it’s activated, these guys can actually migrate from joint to joint. So they can migrate from the hand joint on one side to the hand joint on the other.
And this is why we get symmetrical arthritis. In rheumatoid arthritis, we also can find t cells in the area. In the synovium, t cells make up about 50% of the immune cells in this area. So they’re very important in the pathophysiology. T cells promote inflammation, essentially, and they can secrete interleukin 17, which will promote macrophage activity, as well as stimulate the fibroblast like synoviocytes.
The T cells also help in the expression of rank l, which will stimulate osteoclast for bone erosion. We also find plasma cells in the area, and plasma cells only make up a small majority, about 5% of the immune cells, and they essentially assist in inflammation through cytokines as well as through antibodies. Now, in the fluid, in the synovial fluid, not in the synovial membrane.
In the synovial fluid, we can find neutrophils and neutrophils. They essentially produce proteases and reactive oxygen species, which will essentially cause bone and cartilage degradation, erosion. So they contribute to inflammation. In the synovial fluid, we also find the immune complexes, which is a feature of rheumatoid arthritis. These immune complexes are essentially antibodies that bind to one another, and they essentially promote inflammation.
So those are the cells that we can find in an inflamed joint in rheumatoid arthritis. Again, another feature around this area is that we see angiogenesis. Also the cytokines that are produced by all these cells. They help increase vascular permeability and the expression of adhesion molecules on the vasculature, allowing for these immune cells to migrate into the joints.
But where do all these cells come from? Why do they migrate into these joints and cause rheumatoid arthritis? Well, as I mentioned, we don’t actually know, but there are a few theories out there. So let’s go to the pre rheumatoid arthritis phase before a person has rheumatoid retinal arthritis.
And there are many possible things that could contribute to the development of rheumatoid arthritis. These include genetics, epigenetic modifications, smoking, a bacteria called porphyrimonus gingivalis, which can lead to gingivitis. Essentially these things, they can cause modification of otoantigens. What do I mean by modifications of otoantigens? It.
What I essentially mean is modification of your own antigens to make it seem foreign to the immune cells. So these things can lead to modifications of your own antigens, leading to an immune response. And the modifications of autoantigens include what’s known as citrullination. So not only this, things can occur in the joints, such as you can have synovial injury or hyperplasia, or you can have infection within the joint, and this will trigger cytokine release, and it will cause inflammation.
This inflammation that occurs in the joints can also lead to modification of autoantigens. So modification of your own antigens, making it seem foreign. And this also includes citrullination. So because you have modifications of your own antigens, this will be recognized by antigen presenting cells, and it will essentially activate the antigen presenting cells to initiate an immune response.
The antigen presenting cell will migrate to the lymph nodes, where here I’m drawing the lymph node. Remember, the lymph node here is in green. And within the lymph node we have the germinal center, where we have b cells. Anyway, the antigen presenting cell will activate t cells here in the area. So we can have CD four t cell activation. And when the t cell is activated, the CD four t cell, it can activate then b cells in the germinal center.
And this can be through co stimulation. When the b cells are activated, they will begin to proliferate, they’ll begin to class switch, and they will become plasma cells. Then plasma cells will then produce o, two antibodies. They will produce the antibodies against your own antigen, essentially.
So then what? Well, you have now CD four t helper cells, and then you have the antibodies and the plasma cells, and they will also have homing receptors and stuff like that, which will allow them to migrate to joint tissue. So that is how they move into the joints in rheumatoid arthritis. So I hope that made sense. Now, it’s important to talk about the antibodies because they are important feature in rheumatoid arthritis.
We have two main antibodies found, and these are, we’ll look at one of them at a time. So the first one is the rheumatoid factor, which is an igm antibody, and it’s present in 75% of people with rheumatoid arthritis. What these guys do is that they target Fc portion of igg antibodies. So the constant region, and they essentially are the ones that form the immune complex and can deposit in the synovial fluid.
The rheumatoid factor not only forms immune complexes with itself, but with the IgG as well as complement proteins, so it will promote inflammation. The second antibody is the antisitrullinated protein antibody. Now, these guys, as the name suggests, they target citrullinated proteins. These are things such as fibrine and filigrine. Now, they target citrullinated proteins.
What are they? Well, citrullinated proteins are essentially proteins who have arginine residues that have been converted to citrullinate. And this sort of change makes it seem foreign to the body. And that is why when we have modifications of our autoantigens, such as citrullination, our body thinks it’s foreign. And unfortunately, in our joints, we have these sort of tissues. So therefore, that’s how this antibody contributes to the pathophysiology.
But essentially, these rheumatoid factor and anticitrullinated protein antibodies, they’re important in helping diagnose rheumatoid arthritis. Not everyone has rheumatoid factor, but the anticitulated protein antibody, it is a lot more specific for rheumatoid arthritis. So I hope that all made sense. Now, it’s important that we talk about the extraarticular involvement within rheumatoid arthritis.
So what I’m talking about is involvement of other organs around the body and how rheumatoid arthritis causes problems there, too. So these extraarticular involvement is a result of the cytokines produced within the joints and stuff. And these are mainly tnf alpha, interleukin one and interleukin six. So, within the blood, we have increase in inflammatory cytokines, and they essentially contribute to many things around the body.
For example, in the skin, they contribute to the nodule formation in the liver. Because of these cytokines, the liver will begin producing more CRP or ECR proteins, which are inflammatory markers, as well as the liver will produce a lot more hepsidin, which will contribute to anemia in rheumatoid arthritis. Cardiovascular involvement. Well, these cytokines and this inflammation that’s occurring will actually promote arthrogenesis.
So plaque formation, and it can also lead to promote myocardial infarction as well as stroke, neurological involvement include fatigue and depression and these can be attributed to anemia. Bone involvement is very serious in rheumatoid arthritis, sorry, musculoskeletal involvement. So these include osteopenia, which can lead to osteoporosis in the muscles.
The inflammation can lead to insulin resistance, which can result in muscle weakness and also bone marrow involvement. We can have thrombocytosis, which is a lot of platelet, which can contribute to the plaque formation, the thrombos formation, as well as we have anemia. So I hope that made sense and I hope you enjoyed this video. So those are the extraarticular involvement of rheumatoid arthritis.
You also have lung involvement, such as plural fusion and lung infection, but this can be attributed to the treatment used for rheumatoid arthritis, which involves glucocorticoids and as we know, glucocorticoid suppresses the immune system. I hope you enjoyed this video. We looked at the clinical manifestations, the hand involvement, the pathophysiology, the causes, potential causes, as well as the articular manifestations of rheumatoid arthritis. Thank you for watching. Bye.
Rheumatoid arthritis, or ra, is a condition that causes swelling and pain in joints. It’s different from other kinds of arthritis. It’s a lifelong condition. RA causes inflammation, swelling, redness, and pain, and it can damage the joints. Every person has an immune system to be able to fight infections such as bacteria or viruses. In Ra, the body’s immune system begins to attack its own joints and can sometimes attack other parts of the body.
No one knows exactly why Ra can begin in any joint, but can eventually affect all of them, wrists, hands, knees, ankles, shoulders, leading to stiff, swollen, or painful joints. The lining inside of the joint is called synovium. In Ra, the synovium becomes inflamed and swollen, causing pain and stiffness. There is no cure for Ra, but the drugs discussed in this program can slow down the disease and help you feel better.
If left untreated, RA will get worse. In fact, without treatment, the inflammation will continue to damage and eventually destroy the joints, organs, and other parts of the body. Occasionally, the inflammation can affect other organs, such as the eyes or lungs. Any organ can suffer, and Ra can even cause disability, such as difficulty using your hands or problems standing and walking.
RA is a serious condition. It requires treatment and monitoring by a doctor to prevent additional problems. Hey, how’s it going? I am really glad to see you. Why? What’s going on? I started reading all this stuff and there’s really a lot to decide. Oh my. Like what? Well, a lot of it has to do with the drugs they use to treat this. Let’s just look at this. Wow. I see what you mean.
I mean, it’s nice they summed it up like this, but it is a pretty long list. Yeah, I’m not even sure what I’m supposed to know about all these drugs. Medicines are the main treatment for Ra. They relieve pain and reduce the swelling in joints. Most people with RA need to keep taking their medicines for life. This guide talks about two kinds of RA medicines, demards and steroids.
Demards stands for disease modifying antiromatic drugs. These medicines relieve inflammation and pain, and they also slow or sometimes stop the changes in your joints. There are many different DmaRD drugs. Some are in pill form, some are injections or shots, and others are given intravenously or iv through a needle in your vein. There are at least ten different demards.
They each have a generic name and one or more different brand names. You can find a list of all of the current ones in your guide. One of the standard demards that’s often used is called methotrexate. It’s a pill, and for many people, it works as well as other Dmards that are given by shot or intravenously or iv. Most of the demards that are given either as injection or by iv are a newer class of drugs that are also sometimes called biologic demards because they have a different way of acting than standard demards, like methotrexate.
Sometimes doctors will prescribe a combination of medicines, one or more standard demards, or a combination containing a standard and a biologic demard. The other drugs we use are called steroids, drugs like prednisone or prednisolone. These are manmade forms of hormones that your own adrenal glands make. These drugs help with joint pain and swelling, and there is some evidence that, like Dmards, they may slow down the damage to your joints.
Your main treatment will be one or more of the Dmards and steroids as needed when recommended by your doctor. Finally, your doctor may also prescribe a nonsteroidal antiinflammatory drug, an nsaid like ibuprofen or naproxen, to help with the pain and inflammation. For many patients with rheumatoid arthritis, it may take some time to find the best combination of medicines.
If one medicine or combination of medicines isn’t working well, your doctor may switch you to other drugs or add more medications to the mix in order to achieve the best relief. Your doctor will work with you over time to find the drug or combination of drugs that it was about four years ago when I got my first symptoms of ra. I started feeling like every joint in my body was sore.
I mean, I couldn’t even walk because of the pain. It was almost impossible to walk downstairs most mornings, and leaving my house for the day was a nightmare. When I saw my family doctor about all this pain, she really didn’t know what it was. I took some pain pills, but they didn’t help much, and I felt like my body really started to swell up. My doc told me that I should see a rheumatologist, one of those docs that specialize in joints, and she prescribed some medication called methotrexate.
I was doing okay with the methotrexate. My doctor told me to take six pills that I took all at one time, once a week. And he also gave me some other pills called prednisone. After about a year, this medication just wasn’t doing the trick. So my doctor upped the methotrexate to ten pills a week. I also needed to get blood tests to be done with the treatment to make sure that my body was adjusting and handling the meds okay.
I took methotrexate for two years with no side effects. After that, I started to have liver problems, and my doctor thought that maybe it was caused by the pills. So he put me on four pills only. But even then, I still continued to have liver problems. Then my doctor recommended an injection he called antitNf, which is a biologic therapy. I’m always scared to start taking a new drug, especially when it’s a shot, so I was a little nervous about it, especially because I needed to inject myself.
The doctor then explained to me how to do it. I also wondered if there was anyone out there who had had some good results while they were on the shots and without too many side effects. He said there were many other patients who were using these injections and were happy with their improvement. I’m thankful that I have a doctor who is willing to go over my concerns and all my questions.
The injections have done wonders for my pain and the severe joint inflammation that I had. But these meds have to be taken very seriously, so I continue to get blood checks to make sure everything is fine. Remember, there are two main types of medications for RA, demards and steroids. However, taking other medications may be needed to feel better. One of the Dmards will be your main treatment.
All of the DmarD drugs work and they can slow down the disease and relieve pain, but it’s hard to predict which drug will work best for any one person. About 65 out of 100 people need to change their RA drug at some point, either because it isn’t working well enough or because of side effects. Given the many dmards available to treat RA, there are some factors that might influence the choice that you and your doctor make.
One factor is how the medicine is taken. Some dmards are pills, and pills are certainly easier to take than those that have to be injected. For most people, some of the pill forms have to be taken every day. Others are taken once a week. Cost is another factor, and for the most part, the pill forms are less expensive. Most people can start with a pill, but if that isn’t working, the doctor may change to a Dmard that’s given by injection or shot.
Most people give the injections to themselves at home. Some of the demar shots are only needed once or twice a week, and still others are only needed once every two weeks. Other Dmards, like abatticept, infleximab and rituximab are given intravenously or iv. That’s an infusion that goes into a vein. This is a treatment that you get at a clinic or your doctor’s office, but most people only need to have it once every few weeks.
Demards do not start working right away. It may take weeks or months to start working. So you may need other medications like steroids or pain medicines. In the meantime, the steroids that are used are not the same ones as you hear about athletes misusing. Remember that steroids may slow down the damage to your joints that is seen in x rays, and they may help to alleviate the symptoms.
But they can have side effects if they’re used for a long time. So your doctor will probably try to use them sparingly only when you need them. All of these medicines can help you, but they are powerful, so you’ll need to be careful about certain things. One of those things is infections. Remember that RA is caused by your immune system attacking your own tissues.
So all of the drugs we use are designed to suppress your immune system to make it less active. But since your immune system also protects you by fighting infections that suppress, it can put you at higher risk of infection. In other words, it’ll be easier for you to get infections when you’re elephants. Go to Home