Thanks to Ivy League research that replaces old, tired, worn-out joints without even breaking the skin…
Using this weird “jelly” discovered in a tiny remote Japanese village.
Think it could work for you?
Test it out for yourself here:
This morning water trick REMOVES joint pain

The word osteomyelitis can be broken down. Osteo refers to bones. Myel stands for myelo and relates to the bone marrow. And lastly, itis refers to inflammation. So osteomyelitis is an inflammation of the bone or bone marrow, and it typically results from an infection. Normally, if we look at a cross section of a bone, we can see that it has a hard external layer known as the cortical bone, and a softer internal layer of spongy bone that looks like honeycombs.
There’s also another layer called the periosteum that covers the cortical bone like the lamination of a basketball card. And that’s where the muscles, tendons, and ligaments are attached. If we zoom into a cross section of cortical bone, we can see that it has many pipelike structures called osteons running through the length of the bone. Each pipe has an empty center called a herrsion canal, which contains the nerves and blood vessels that supply the osteon.
At the outer border of the osteon is a ring of cells called osteoblasts, which synthesize bone. Along with these cells are osteoclasts that break down bone. In bones like the long femur, the tips are called the epiphysis, while the shaft is called the diaphysis. Between them, we have the metaphysis, which contains the growth plate, the part of the bone that grows during childhood. In osteomyelitis, microorganisms such as bacteria reach the bone to cause an infection in a few different ways.
Bacteria particularly affect certain high risk individuals, like those with a weak immune system and those with poor blood circulation due to uncontrolled diabetes. In fact, a major way that bacteria reach the bone is through the bloodstream, and that’s called hematogenous spread. For example, this might happen in a person who uses contaminated needles to inject drugs or in individuals undergoing hemodialysis that may be contaminated by a bacteria or even through the dental extraction of an infected tooth.
Through the bloodstream, the microorganisms may reach specific places in the body, and this mostly depends on the age of the person. In older adults, for example, the microorganisms may reach the vertebrae and cause vertebral osteomyelitis. This usually affects two adjacent vertebrae and the intervertebral disc between them. In children, the metaphysis of long bones like the femur is commonly affected. The second way that bacteria cause osteomyelitis is through trauma.
For example, in an open fracture after an accident, the bone may get exposed to the outside environment and come into direct contact with bacteria. A third way is during surgery when there’s bacteria that’s introduced into the bone. A fourth way is when an infection spreads from one area like cellulitis, which is an infection of the dermis layer of the skin, to an adjacent area like the bone, and this is known as contiguous spread.
There can also be combinations of these, for example, when a prosthetic joint becomes contaminated with bacteria during surgery, and then that bacteria contiguously spread to nearby bone. Another example is when people with diabetes mellitus develop a severe vascular compromise. A small trauma to the foot can lead to the formation of a foot ulcer, which then becomes infected and spreads to the nearby bone.
Now, once the bacteria reach the bone by any of these roots, they start to proliferate. This alerts nearby immune cells, specifically dendritic cells and macrophages that try to fight off the infection. This represents the acute phase of the disease and occurs over a course of weeks. The immune cells release chemicals and enzymes that break down bone and cause local destruction. Usually, acute osteomyelitis comes to a resolution, meaning that the immune system eventually destroys all of the invading bacteria.
If the lesion is not that extensive and there’s viable bone, the osteoblasts and the osteoclasts begin to repair the damage over a period of weeks. However, in some cases, the process turns into chronic osteomyelitis, lasting months to years. In that situation, the affected bone sometimes becomes necrotic and separates from the healthy part of the bone, and that’s called a sequesterum. At the same time, the osteoblasts that originate from the periosteum may form new bone that wraps the sequesterum in place.
This is called an involve. Occasionally in both acute and chronic osteomyelitis, the inflammation may involve the periosteum. The periosteum is loosely attached to the compact bone, especially in children, so the two layers can separate and allow an abscess to form between them. That sort of an abscess tracks along the periosteum, lifting it up away from the compact bone. The infection can also spread further to involve a nearby joint, particularly the knee or hip joint, in young children, as well as overlaying muscle skin and even get into the blood vessels, causing thromboflabitis.
Many microorganisms cause osteomyelitis, but the most common is Staphylococcus aureus, a grape looking bacteria that lives on the skin. It can invade the skin and spread contiguously to the bone, or it can reach the bone through the bloodstream. Another one is salmonella, a rod shaped bacteria that particularly affects individuals with sickle cell disease. Unfortunately, individuals with sickle cell disease are therefore at risk of getting both Staphylococcus aureus as well as Salmonella infections.
Another pathogen is Pasteurella multicyda, a pill shaped bacteria. It usually spreads from the skin to the bone from a bite or scratch from a cat or dog. Now, acute osteomyelitis typically causes pain at the site of infection as well as fevers. Depending on the location, it may affect use of the bone. In chronic osteomyelitis, there can be prolonged fevers and weight loss due to the chronic inflammatory state.
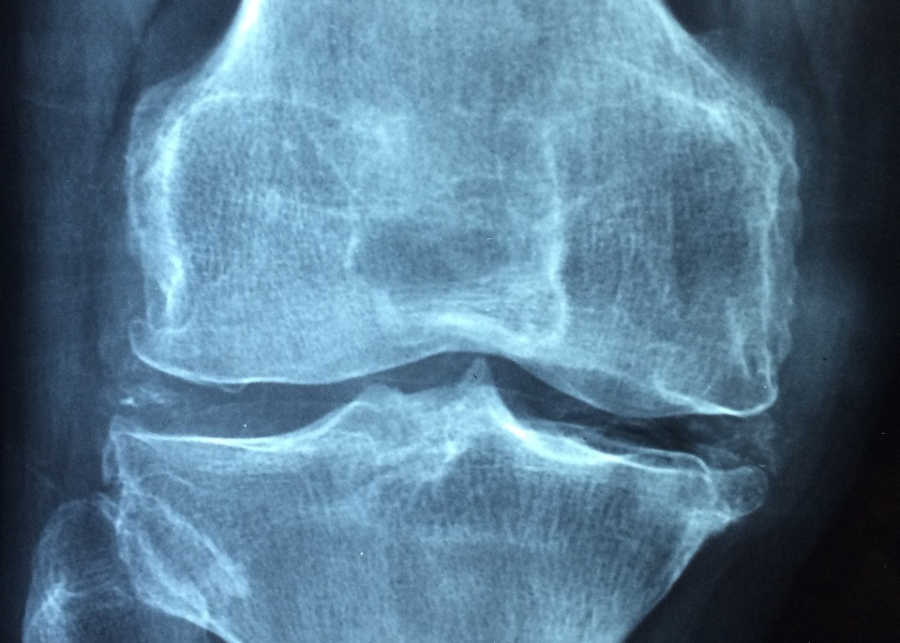
Osteomyelitis is usually diagnosed by using a complete blood count or CbC, which shows an increase in white blood cells as well as an elevated erythrocyte sedimentation rate or ESR, and creactive protein or Crp. These are both non specific markers of inflammation. Now, in addition, sometimes an x ray is done and it might show thickening of the cortical bone and periosteum as well as an elevation of the periosteum.
Other findings may include loss of the normal architecture of the bone, especially of the trabecular architecture. There’s also osteopenia or loss of bone mass that becomes evident when more than half of the bone matrix is destroyed. Typically, a bone scan or MRI is done to help confirm the presence of osteomyelitis and to identify a possible abscess. When possible, a bone biopsy is also taken to help culture and identify the pathogen responsible as well as confirm the diagnosis.
Now, treatment typically involves weeks of antibiotics directed at the organism causing the infection. If there’s an abscess, particularly a vertebral abscess causing neural compression or spinal instability, then surgery may also be required. In addition to draining abscesses, surgery is often needed to remove any necrotic bone, particularly in chronic osteomyelitis, the sequestrum has to be removed. All right, as a quick recap osteomyelitis is a bone infection in which the symptoms are inflammation, fever and weakness. Staphylococcus aureus is the most common pathogen responsible for osteomyelitis and the most common form of infection is through the bloodstream.
Osteomyelitis bone infection osteomyelitis is an infection of the bone. It may be an incurable disease. So what really happens with bone infection or the osteomyelitis? Usually the bacteria causes the infection in the bone. Staph aureus is the most common organism in adult the leukocytes, which is the white blood cells, are attracted to the area and secrete enzymes in an attempt to kill the bacteria. The blood flow to the area is decreased and a devitalized necrotic bone is formed and that is called the sequestrum.
Sequestrum is an infected dead bone resulting from osteomyelitis and here there is a presentative example of a sequesterum which is the nitus of infection. Haversian canals surround blood vessels and nerve cells throughout the bone. The sequesterum has no connection to the normal bone through the Havergian system and because this sequesterum is evascular or a dead piece of bone, antibiotic cannot reach the sequester or the bacteria.
In fact, the bacteria enters the bone cells and hides inside the bone cells. Antibiotics alone may not help due to difficulty in penetrating the necrotic area. The invulcrum is a new bone formation around the sequesterum. The body is trying to seal off the infection by forming a new bone. The sequesterum will drain through a sinus and the draining sinus is called the kulwaka. Biopsy of the sinus is not representative of the infection.
Multiple deep samples, peripherally, bone biopsy and cultures are needed. Biopsy of the sinus is important in long standing cases of osteomyelitis. Throughout the formation of squamous cell carcinoma. What are the associated medical conditions? Dialysis, malnutrition nutrition is an important part, diabetes, IV drug use or, if the patient is immunosuppressed, unusual organisms. For osteomyelitis. In sickle cell anemia, patient may get salmonella however, staph aureus is the most common in patient with iv drug use.
Acromiclovicular or stenoclavicular joint infection patient may get pseudomonas patient may get pseudomonas through a punctual wound through the shoes immunosuppress patient and patient in parental nutrition may get fungal ostomyelitis. In children, isenophilic granuloma, ewing sarcoma and acute osteomyelitis may resemble each other. Patient may come with pain, fever, tenderness of the area and also the patient may have an increased remitation rate and leukocytosis osteomyelitis can also be confused with a healing fracture or with a benign or malignant tumor.
Sometimes a biopsy is necessary for the diagnosis. Only 50% of chronic musculoskeletal infection will have elevated inflammatory markers. Classification of osteomyelitis acute, usually within two weeks chronic after several months subacute from four weeks to several months there is cerny major classification system three types of patients and four types of bone infection. Three types of patients a is healthy b compromised can be locally compromised like the patient has sinus tract or free flaps or decreased blood supply or systemically compromised the patient with comorbidities and the c is severe.
Systemic compromise the host in whom treatment will lead to greater morbidity than the infection itself. Then the types of bone infections there are four types of bone infections. Number one medullary number two superficial number three localized defect with a stable bone number four diffuse infection with involvement of bone stability. Principles of surgical treatment for osteomyelitis treatment of osteomyelitis is usually a combination of surgical debridement of the necrotic nonviable tissue plus administration of culture specific antibiotics.
One, open the enveloperum, which is the new bone two, remove the sequestrum, which is the dead bone three, tocerize the bone. Make sure a pathological fracture is not created. Stabilize the bone if needed. External fixator is usually preferred. Fill the cavity with bone chips, cement or muscle flap if needed. Intravenous antibiotics are usually given for a period of six weeks and it is usually organism specific. Recurrence of the infection is high.
It occur in about 30% of cases. Important topics Mercer osteomeralitis temperature more than 38 wbcs count more than 12,000 hematocrit less than 34% three, active protein more than 13 these four independent predictors differentiate between MRSA and methylastomyelitis with 92% chance of having Mersa if all the four are present. If you have Mersa, give vancomycin or clindamycin and in Mercer you will have a higher incidence of DVT than other causes of osteomyelitis.
Older children eight years old or more with Mersa ostromyelitis and CRP more than six has a 40% incidence of DVT on presentation. The presence of pantom valentine leukocydin gene encoded in strains of Mercer bacteria may explain the deep venous thrombosis. Understanding the principles of treatment of chronic ostomyelitis, careful workup and staging of the bone and the host. Utilizing the cereal classification is important to develop a successful treatment plan.
The principles of treatment of chronic osteomyelitis includes so you do debridement. First you will do dead space management, usually by putting cement spacer with antibiotics. Then you will do soft tissue coverage, and then later on you remove the cement spacer. Then you’re dealing with the bone defect, usually by adding bone graft.
And during the treatment you’ll figure out about the stability of the bone and you’ll add external fixture if needed, the muscular technique which is called induced membrane antibiotic cement spacer, followed by the soft tissue coverage and we do stage bone graft at six to eight weeks later, debt induced membrane then later we do stage bone graft. The membrane secretes bmp, two bone morphogenic protein and vegF, and other growth factors, which peak around four weeks after membrane induction. Thank you very much. I hope that was helpful.
bones are usually healthy and strong and they sustain us with movement, et cetera. However, due to some form of trauma, vitamin A deficiency deficiency, low bone density or being old, bone fractures can occur. Bone fractures can lead to tears in blood vessels which carry nutrients to the bone, which will cause some problems.
But our body obviously has some mechanism to repair bone fractures. Now, bone fractures itself can be categorized into four parts can be classified by the position of the bone ends. After a fracture can be classified of the completeness of the fracture, the break, the orientation of the break, or whether the bone ends penetrate the skin. So position of the bone ends can be classified under two types. In nondisplaced, the bone’s position does not move.
However, in displaced, as you can see by this diagram. If I draw it, okay, you can see that the bone moves and this is displaced because the bones are displaced up to the fracture. The completeness of the break essentially means whether the bone completely fractured or incompletely fractured. So whether it incompletely doesn’t break off or it completely breaks off. Now, the orientation of the break, what it means that whether the fracture is on a vertical axis or a horizontal axis, also known as linear or transverse penetration of the skin, is obvious.
A fracture that penetrates the skin will cause a compound fracture, and one that does not penetrate the skin will cause a simple fracture. Okay, let’s just learn more about bone fractures. Let’s just say a kid fell down and broke his fibula or tibia, for example. So now what happens to the bone? Let’s zoom into the bone and learn how the fracture repairs itself. So here is a bone. A typical long bone contains the periosteum, which wraps around the bone.
This is the fracture. We have the compact bone and the hollow tube which is formed by the compact bone. And we also have the spongy bone. We have blood vessels here and blood blood is formed and accumulates in the body. This is just after the fracture. However, a few seconds minutes after the fracture, we have major swelling. Here’s a fracture again. This stage is known as the hematoma stage, or where the hematoma formation begins.
And essentially the hematoma formation is when blood accumulates, forming the hematoma. And this causes a death of some cells and swelling and pain associated with the area. And as you can see, the vessels are damaged here. After a few days, the bone will go to the second stage, known as fibrocartilogenous calla stage, or the fibrocaltogenous callus formation, the soft callus formation. So the blood vessels here are regrowing.
We have new blood vessels forming, and a type of meshwork from granulated tissue forms the callus. And also outside the fracture, where the perostinium is, we have the external callus being formed. So the granulation tissue fills in the gap where the fracture is and rejoins the fracture, the fractured bones together. And this is what the soft callus essentially does. Then after a few weeks, the fractured bone will enter the third stage, which is the bony callus formation stage.
Now, this stage, the bony callus formation stage, is when the soft callus previously formed, will then become a bony callus. And we have new blood vessels here and here. Now we have the bony callus, which is formed with the help of also other tissues in the area. So soft callus converts to bony callus in this stage. Then after several months, the bony callus will remodel to become fine bone. So this is the bone remodeling stage, where the bony callus is remodeled to become strong new bone.
So healing occurs, and the compact bone is laid down, and osteoblastic activity also is increased during this stage. So essentially, the previously fractured bone is now completely healed after the four stages. Hematoma stage, fibrocultilogenous callus stage, the bony callus stage, and the last stage, which is the bone remodeling stage. Let’s talk about osteomyelitis now, which is related to bone fractures. So what is osteomyelitis? Well, osteomans, bone and mellitus means marrow, and we’ll see the relationship why.
Osteomyelitis is when a bacteria, specifically a staphylococcus strain, can infect a bone during a bone fracture or through the bloodstream. And once this bone has been infected, the person will start feeling severe pain, sweating, and also swelling of the bone injured site. And what this bacteria usually infects are long bones, the ends of long bones. And at the ends of the long bones, the bacteria will cause necrosis of the bone cells. So the bone cells begin to die.
There’s also pus being formed. And essentially, this previously strong bone will become weak. Not only that, but if this condition is not treated as soon as possible, the osteomylatis can become chronic and a lot of bone cells can begin to die. And this can have serious consequences. And this black patch is the infected area, for example. And the cause of osteomyelitis, as I mentioned, is staphylococcus, but particularly this type, staphylococcus iris.
So once this bone has been infected, there are some serious changes. First of all, pus can be formed by the infected area because of immune cells trying to neutralize this problem. So pus formation, and it moves out of the cavity and pushes the peritoneum out. And essentially, after a while, what this would do is that new bone formation could possibly occur because the bone cells around that area will think that the body wants to create new bone.
But essentially, osteomyelitis actually causes bone death, specifically at the ends of long bones. And that is why osteomyelitis is a very serious condition. So that concludes this video on bone fractures. We talked about bone fractures, the types of bone fractures, how bone fractures are healed, and we talked a little bit about osteomyelitis. I hope you actually enjoyed that short video. Please comment, like and subscribe. Shanghyo. Go to Home